「結局、どのCBDグミが1番満足できる?」
こんな悩みを抱えていないだろうか。
この記事では、今までに10種以上のCBDグミを経験した私が、心からおすすめできるCBDグミをランキング形式で紹介する。
つまり「誰でも満足できる”当たり”のCBDグミ」をここで紹介できると自信を持っている。
では、早速見ていこう。
おすすめのCBDグミ7選
今から紹介するCBDグミのランキングは、下記の基準で作成した。
・手頃な価格かどうか
・フレーバーは豊富なのか
・安全性に優れているのか
つまり、満足度が高い順でランキングしたということである。
ちなみに、ランキング作成の話し合いには、6時間を費やした。
適当に順位はつけてないので、このランキングを参考にして後悔することはまずないはずだ。
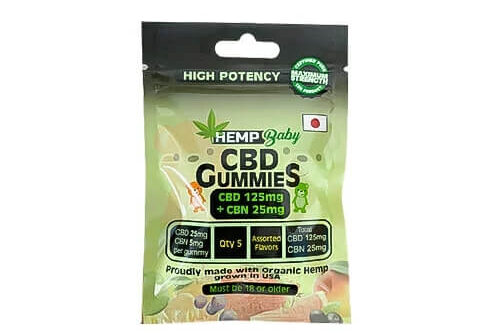
1位 Hemp Baby 1粒25mg版
2位 CBDfx
3位 プラスウィード
4位 グリーンブルドッグ![]()
5位 CANNA NANO
6位 Hemp Baby 1粒15mg版
7位 CBD LIVING
1位 Hemp Baby 1粒25mg版
| 内容量 | CBD含有量 | フレーバー | 価格 |
| 5個 | 125mg | 5種 | 1,680円 |
| 25個 | 625mg | 5種 | 7,180円 |
| 50個 | 1250mg | 5種 | 9,800円 |
| 100個 | 2500mg | 5種 | 15,800円 |
Hemp Babyは、CBDグミの中でもだんとつでおすすめできる。
コスパの良さはもちろん、1つのボトルに5種のフレーバーが入っているため、飽きずに楽しめるのが最大の強みだ。
ちなみに私達がおすすめするのは、50個入りタイプである。
ちなみに、フレーバーは下記の5種類。
・レモン
・ソーダ
・オレンジ
・ストロベリー
・グリーンアップル
なお、Hemp Babyには6位で紹介する15mg版もあるのだが、コスパを考えると圧倒的に25mg版の方がおすすめである。
 HEMP Baby(ヘンプベイビー)のグミは満足度がピカイチだった【レビュー】
HEMP Baby(ヘンプベイビー)のグミは満足度がピカイチだった【レビュー】
レビュー:HEMP Baby(ヘンプベイビー)のグミは満足度がピカイチ【ステマなし】
2位 CBD fx

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 8個 | 200mg | 2種 | 1,930円 |
| 60個 | 1500mg | 2種 | 8,930円 |
CBDfxは、「コスパの良さ」が魅力だ。
CBD1mg当たりの価格は1番安く、その上CBDの効き目もしっかりとしているので、満足度は非常に高い。
なおK1王者の武尊選手も愛用しているアイテムであり、Hemp babyに続いて「買って後悔しない一品」という印象がある。
なお、フレーバーは下記の2種類だ。
・アガベベリー
・ミックスベリー
ミックスベリーが無難な味わいであったので、初めての人にはまずミックスベリーをおすすめしておきたい。
 【レビュー】CBDfxのグミはコスパが神だった【あの有名人も愛用する一品】
【レビュー】CBDfxのグミはコスパが神だった【あの有名人も愛用する一品】
レビュー:CBDfxのグミはコスパが神だった【あの有名人も愛用する一品】
3位 +WEED(プラスウィード)

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 25個 | 625mg | 1種 | 5,940円 |
| 50個 | 1250mg | 1種 | 8,640円 |
プラスウィードは、CBDではめずらしい日本のブランドである。
「海外のCBD製品はどうしても不安だ・・」と感じる人にはおすすめであり、お問い合わせフォームもあるため、安心感ではピカイチな印象だ。
しかし、フレーバーは柑橘系の「ネイチャーフレーバー」の1種のみのため、味に焦点を置いている方には残念なポイントになるかもしれない。
とはいえ、満足度が非常に高いCBDグミの1つであることに間違いはない。
 【事実】プラスウィードのグミを30日使った結果【徹底レビューした】
【事実】プラスウィードのグミを30日使った結果【徹底レビューした】![]()
レビュー:【事実】プラスウィードのグミを30日使った結果【徹底レビューした】
4位 GREEN BULLDOG(グリーンブルドッグ)

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 20個 | 400mg | 2種 | 5,400円 |
グリーンブルドッグ![]() も日本のブランドだ。
も日本のブランドだ。
こちらも安心感の点では優れており、CBD含有量は少ないが、フレーバーが2種用意されているため4位にランキングした。
なお、フレーバーの詳細は下記のとおり。
・ブルーベリー
・エナジードリンク
 【断言】GREEN BULLDOG(グリーンブルドッグ)のグミは美味しすぎる
【断言】GREEN BULLDOG(グリーンブルドッグ)のグミは美味しすぎる
レビュー:【断言】GREEN BULLDOG(グリーンブルドッグ)のグミが美味しすぎた
5位 CANNA NANO

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 22個 | 150mg | 5種 | 3,490円 |
CANNA NANO(カンナ ナノ)は、ナノテクノロジーによってCBD吸収率が高くなっているグミだ。
グミという表記だが、チューイングキャンディーに近い食感で、かまなくても口で溶ける感覚があった。
個人的に好きなグミの1つだが、CBD含有量は150mgと少なめい。そのためコスパが良いとは言えないので、その点は注意しておこう。
6位 HEMP Baby 1粒15mg版

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 5個 | 75mg | 5種 | 1,280円 |
| 25個 | 375mg | 5種 | 5,800円 |
| 50個 | 750mg | 5種 | 8,800円 |
| 100個 | 1500mg | 5種 | 14,280円 |
1位で紹介したHemp Babyの15mg版である。
「1個あたりのCBD含有量が少なめのグミが良い」と考える方には、こちらが1番最適なグミである。
やはりHEMP Babyの強みは、1つのボトルに5種のフレーバーが入っていることだ。
毎日楽しく飽きずに使えるため、私達は非常に満足しているグミである。
7位 CBD LIVING

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 30個 | 750mg | 5種 | 8,800円 |
CBD LIVINGは、とにかく質にこだわったCBDグミ・・という印象が強い。
価格は高めなのだが、「ヴィーガングミ」という名前から分かるように、配合する成分にもこだわりを持っている。
品質にとことんこだわりたい人に、おすすめできるCBDグミだ。
格安:20%オフクーポンについて
オトクな情報があるため、共有しておく。
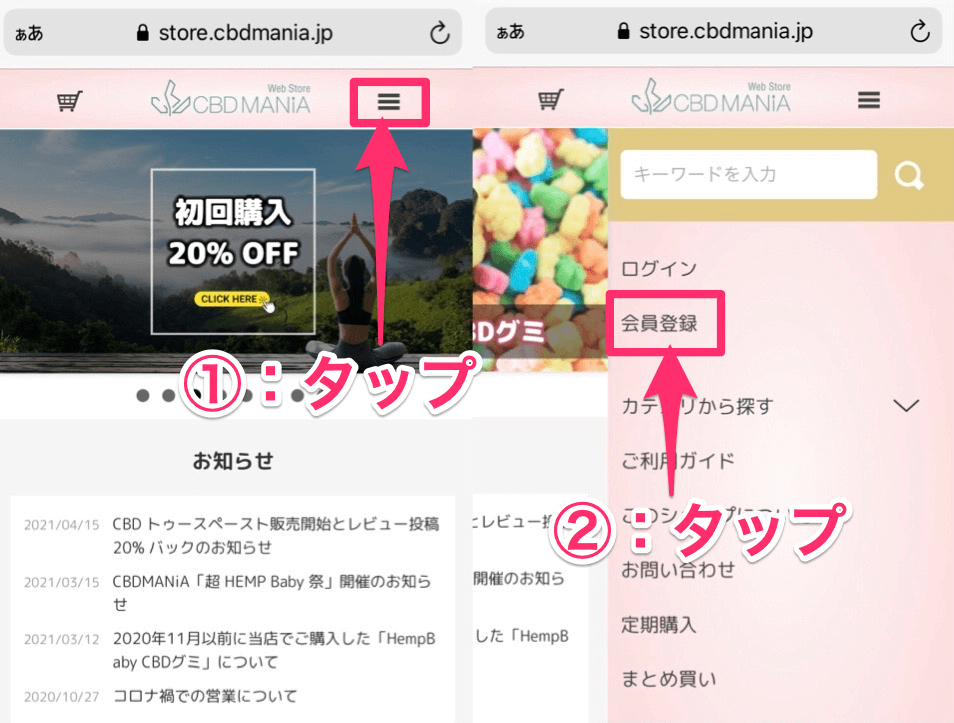
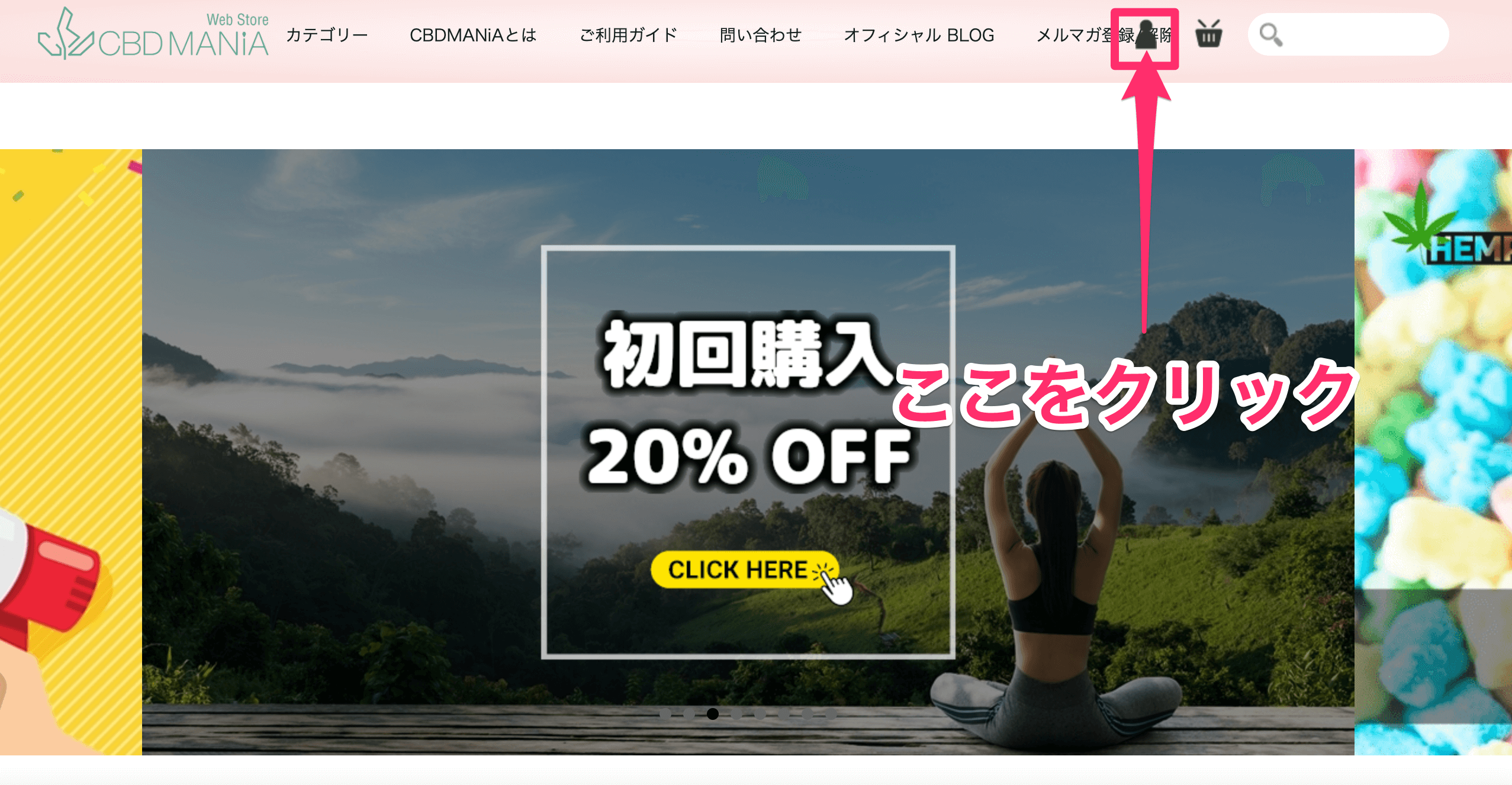
1位、2位で紹介したHEMP BabyとCBD fxは、「CBDMANiA」というオンラインショップを利用することで、初回限定だが20%オフで購入することができる。
CBDは決して高くない買い物なので、こうしたオトクな買い方はぜひ身につけておきたいところだ。
なお私はCBDMANiAのヘビーユーザーであるため、そのクーポンの使い方をここで説明させていただく。
 商品を選択したら、「カートに入れる」をクリックしよう。
商品を選択したら、「カートに入れる」をクリックしよう。
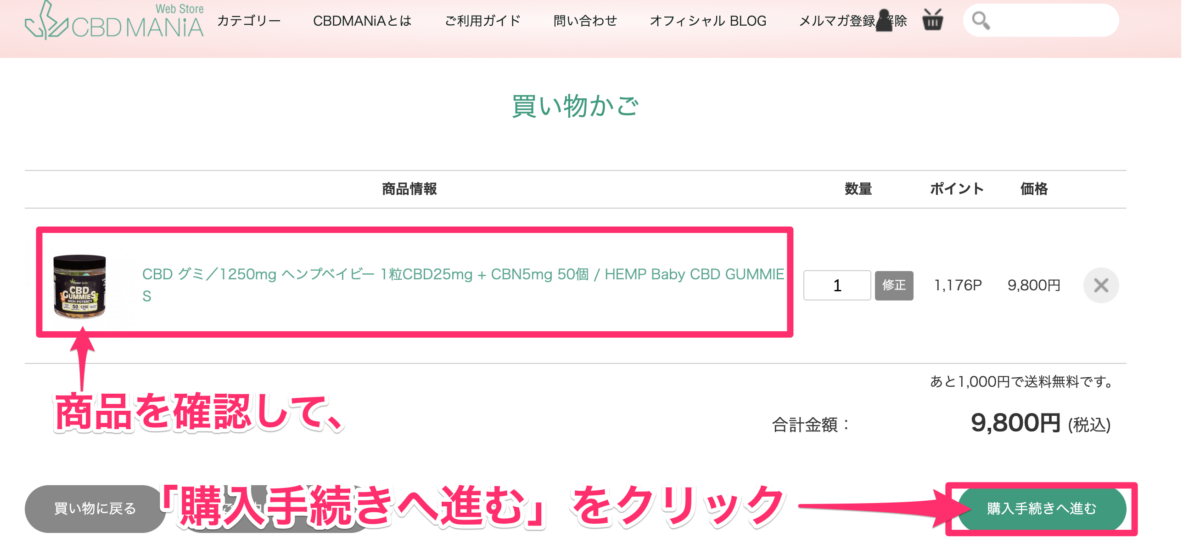 購入する商品が正しいことを確認する。
購入する商品が正しいことを確認する。
そして、「購入手続きへ進む」をクリックしよう。
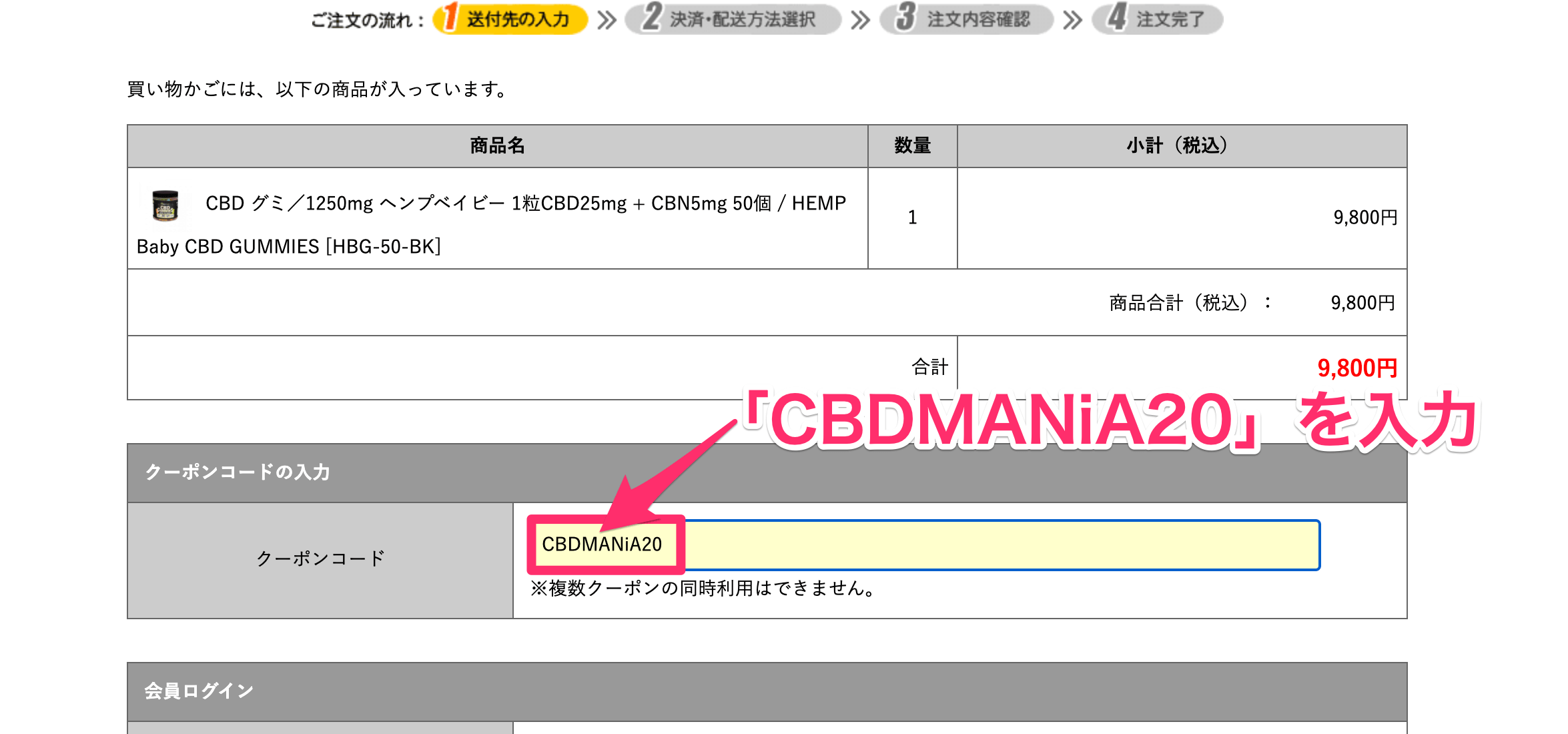 ここで、クーポンコード「CBDMANiA20」を入力する。
ここで、クーポンコード「CBDMANiA20」を入力する。
入力すれば、20%引きが適用される仕組みだ。
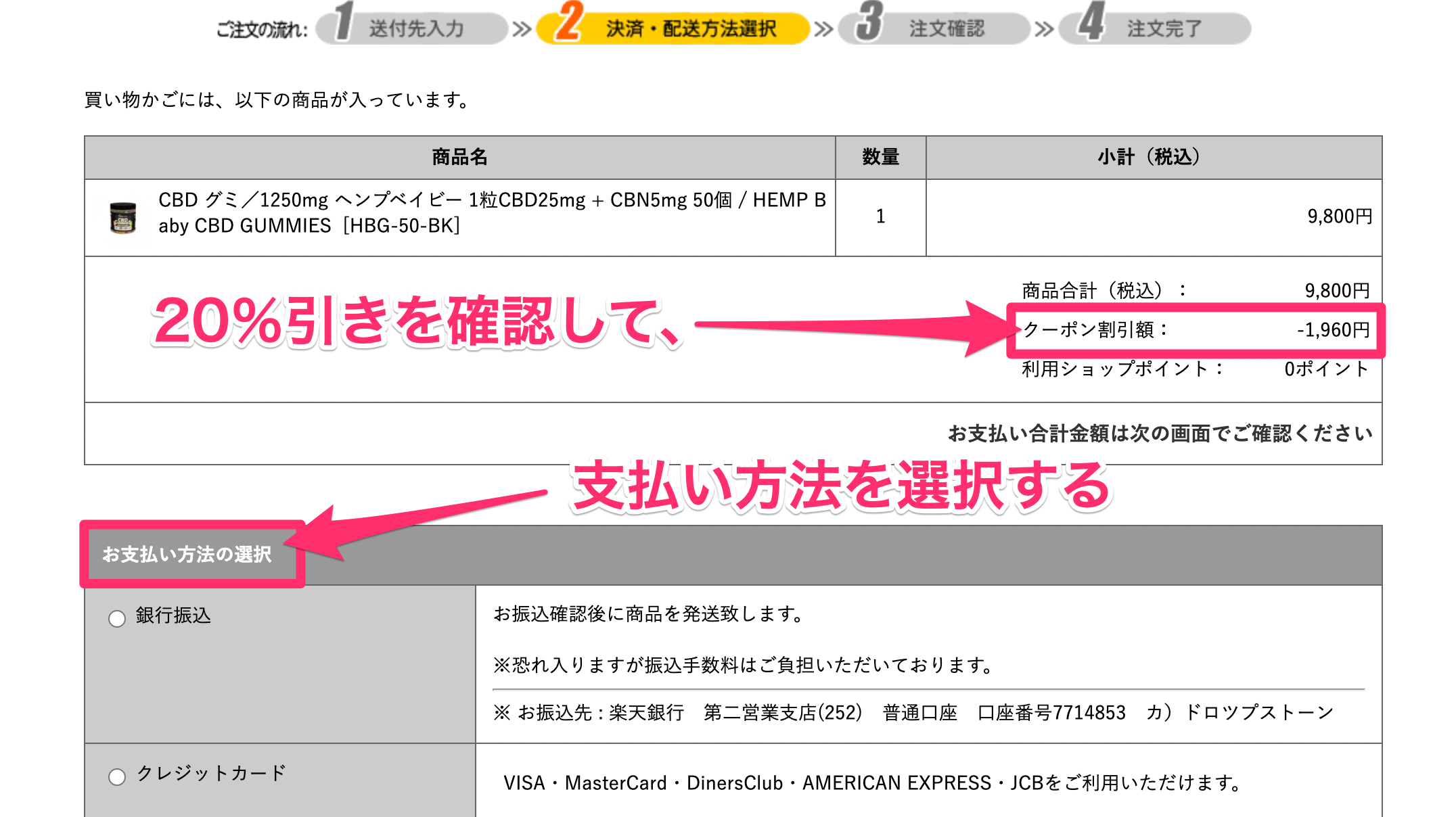 まずは20%引きを確認しよう。
まずは20%引きを確認しよう。
そして、支払い方法の選択へと進んでいく。
なお、支払いには下記4種類が利用可能だ。
・銀行振り込み
・クレジットカード
・楽天Pay
・PayPay
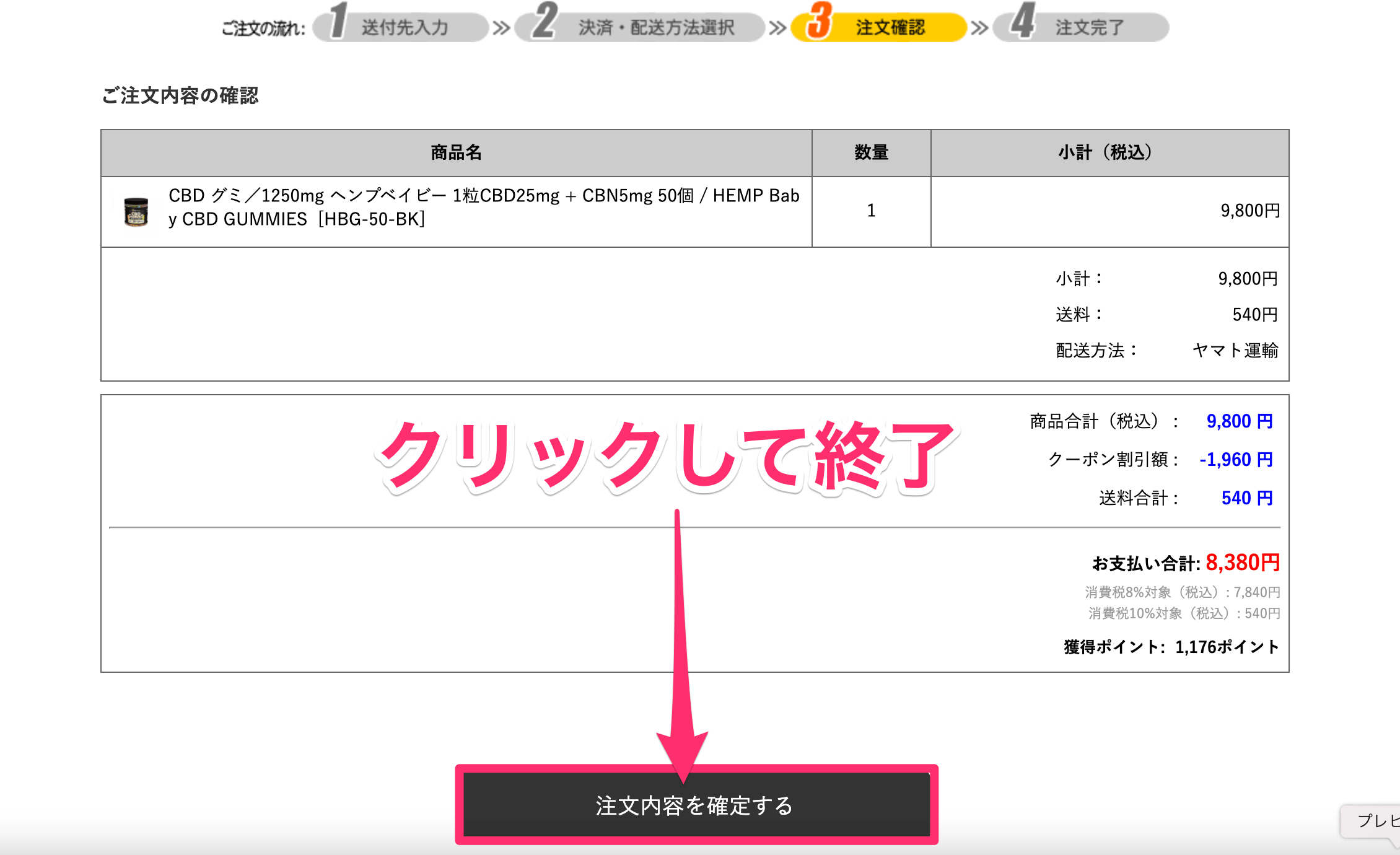 最終確認のあと、「注文内容を確定する」をクリックして終了だ。
最終確認のあと、「注文内容を確定する」をクリックして終了だ。
なお配送は「ヤマト運輸」のため1~2日で届く。
20%クーポンの使い方は上記のとおりだ。
なおCBDMANiA内で販売されているものなら、初回限定だがすべて20%オフになる。
ぜひ、有効活用してほしい。
安いCBDグミのおすすめ5選
ここからは、「価格」だけに的をしぼった、安いCBDグミを5つ紹介する。
CBDグミの「お試し品」を探している方には、価値ある内容であるはずだ。
安い順で、紹介していく。
その①:California Grown 1,080円

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 2個 | 50mg | 1種 | 1,080円 |
内容量は2個のため、コスパは良くない。
しかし、これがCBDグミの中で最安値になるものだ。
その②:HEMP Baby 15mg版 1,280円

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 5個 | 75mg | 5種 | 1,280円 |
内容量が5個なので、California Grownよりは楽しめる。
価格も非常にお手頃なので、お試し品としては最適だろう。
その③:HEMP Baby 25mg版 1,680円
| 内容量 | CBD含有量 | フレーバー | 価格 |
| 5個 | 125mg | 5種 | 1,680円 |
こちらも同じく、5粒入りである。
もしHEMP Babyのどちらかを買うなら、効き目が高い25mg版にしておくべきだ。
ここで400円をケチってしまうのは、非常にもったいない。
その④:CBDfx 1,930円

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 8個 | 200mg | 2種 | 1,930円 |
ジップロック式になっているため、外に持ち出したい人には最適なタイプだ。
スナック感覚でCBDを摂取できるので、こちらも要チェックである。
その⑤:EAST 2,100円

| 内容量 | CBD含有量 | フレーバー | 価格 |
| 8個 | 160mg | 1種 | 2,100円 |
袋が某有名グミと似ているが、そこは気にしないでおこう。
ドンキホーテにも販売されているため、一部の層には人気となっているCBDグミだ。
補足:低価格のグミはおすすめできない
申し訳ない。
「おすすめの安いCBDグミはこちら〜」と紹介しておきながらだが、やはり上記の安いCBDグミは、コスパが悪すぎるので個人的にはおすすめできない。
きっと、そちらの方が下手な失敗をせず、かつ満足度も確実に高まるはずだ。
1年以上のCBD経験から、そう断言できる。
CBDグミの選び方【未経験者へ捧ぐ】
CBDグミを選ぶ時は、以下のことに気をつけると良い。
・内容量
・CBD含有量
・フレーバー
こちらも1つずつ、細かく説明していく。
選び方の基準①:内容量
先ほども話したが、内容量はできたら50個以上のグミを選ぶのが良い。
なぜなら、CBDは継続的に使用するからこそ、より高い効果を感じることができるからだ。
ちなみに私は、期間を空けて1週間グミを食べる、1ヶ月グミを食べるといった生活を送ってみた。
すると、やはり1ヶ月使用した時の方が寝つきの良さなど、いわゆるCBDの効果をより感じることができたのだ。
だからこそ、CBDグミを買うときは50個以上の、つまり「1ヶ月使用できるグミ」を選んで欲しい。
その点を意識すれば、失敗しないグミ選びができるはずだ。
選び方の基準②:CBD含有量
個数と同じくらい、グミ1個当たりのCBD含有量も重要だ。
なぜなら、CBD含有量が少なければ効き目は”うすく”なり、人によっては「ふつうのグミを食べているだけじゃないか?」と感じる場合もあるからである。
なお具体的には、ランキングの1位から3位で紹介した、下記3つのグミが「1粒25mg」の最高タイプなのでおすすめだ。
正直な所、上記3つはハズレのないグミであるため、悩む人はこの中から選ぶのが良いと思う。
選び方の基準③:フレーバー
CBDグミは「食べる」CBDなので、フレーバーの存在も重要だ。
となると圧倒的におすすめできるのが、1つのボトルに5種のフレーバーが入っているHEMP Babyになる・・というのが良く分かると思う。
雑になって申し訳ないが、初めてのCBDグミならHEMP Babyを選んでおくのが1番良い。
CBD含有量も多い、味も飽きない美味しさである、もちろんコスパも優れている・・。
もし私の友達がCBDグミ選びに悩んでいたら、1mmの迷いもなくHEMP Babyをおすすめすると思う。
少し胡散臭くなったが、それくらいおすすめできる「良品」というわけだ。
下手にCBDグミ選びで失敗したくない人は、HEMP Babyが無難である。
なお20%オフクーポンの使い方を分からない人は、「クーポンの使い方」を再度確認して欲しい。
CBDグミに関するよくある疑問
最後に、下記3つの疑問に答えていく。
①:違法性・危険性について
②:CBDグミの食べ方について
③:食べ過ぎの基準について
①:違法性・危険性について
結論から言うと、違法性や危険性などの心配は一切いらない。
というのも、日本で販売されているCBDは、すべて「国」が許可を出している商品だからだ。
また、1年以上CBDを使用している私はCBDによって体調がおかしくなった・・という経験もない。
むしろ、CBDによってQOL(生活の質)は上がったと感じるくらいだ。
まずは体験してみて欲しい。CBDに対して過度な心配は必要ない。
②:CBDグミの食べ方について
グミなので、基本的にはいつものおかし感覚で食べてもらって構わない。
とはいえ、「舌の下」でCBDグミを溶かすように食べると吸収率が上がるので、より効果を感じられるのだ。
ぜひ、意識して欲しいポイントである。
③:食べ過ぎの基準について
1日に1500mgのCBDを摂取しても問題はないというデータがある。
>>引用:Safety and side effects of cannabidiol(英語記事)
つまりCBDグミ(1粒25mg)を1日に60粒食べても、問題はない・・というわけだ。
しかし、そもそも1日60粒のグミを食べるのは常識的ではないため、食べ過ぎの観点はあまり気にする必要はないと思う。
1日に1粒〜2粒。これで充分に効果を感じるはずだ。
まとめ:CBDグミは最強の自己投資である
再度、CBDグミのおすすめを書いておく。
1位 Hemp Baby 1粒25mg版
2位 CBDfx
3位 プラスウィード
4位 グリーンブルドッグ![]()
5位 CANNA NANO
6位 Hemp Baby 1粒15mg版
7位 CBD LIVING
CBDグミは、「食べるだけ」でCBDを体感できるので、非常にコスパの良い自己投資だと感じる。
価格が高いように思えるかもしれないが、コンビニで浪費しているわけではなく、「自分の体のため」にお金を使うので、悪くないはずだ。
私含めて、CBDで救われた人は多い。
私は非常に満足しているので、ぜひこの機会にCBDを体験してみて欲しい。
食わず嫌いはもったいない。